The Heart Rehabilitation Department and nurses at our hospital have developed a unique foot care program. Although foot care guidance itself is not reimbursed by medical insurance, we hope it will contribute to our patients’ health.
1) Target Patients
• Functional venous insufficiency
• Postoperative lower limb venous surgery
• Orthopedic issues such as bunions or flat feet
• Post-thrombotic syndrome (leading to venous ulcers)
*Foot Care Outpatient Guidance
Nurses specialized in foot care take the lead in providing foot care guidance, with all outpatient nurses involved. The significance and process of the foot care program are explained by doctors, and we support patients in incorporating foot care into their daily routines.
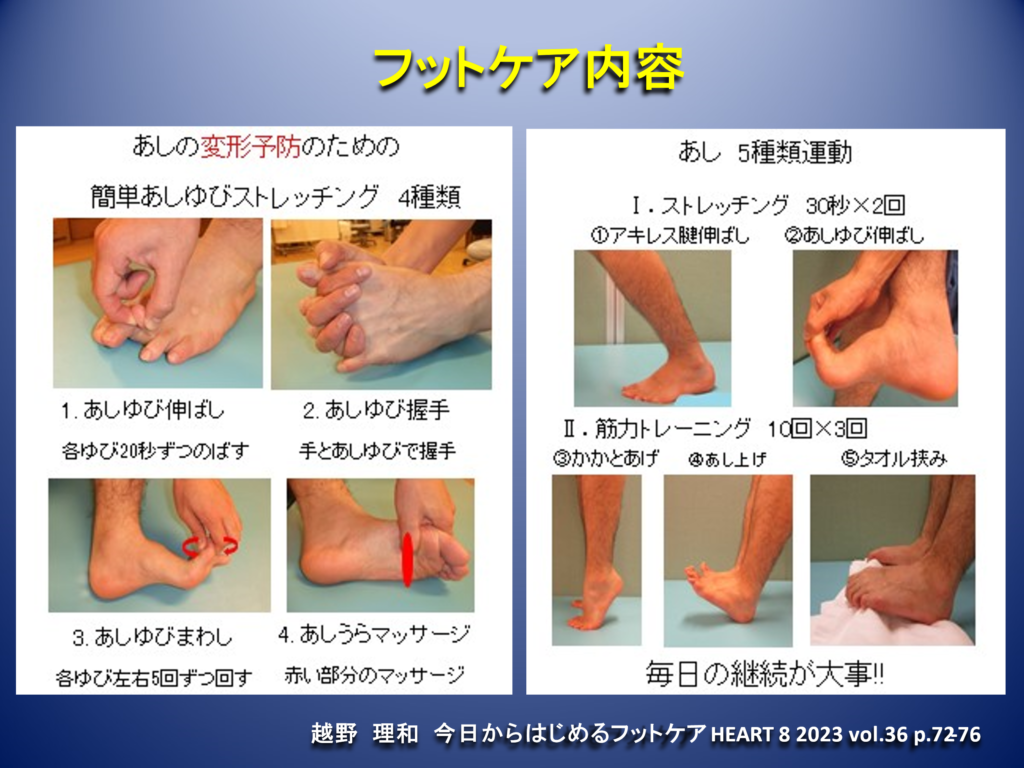
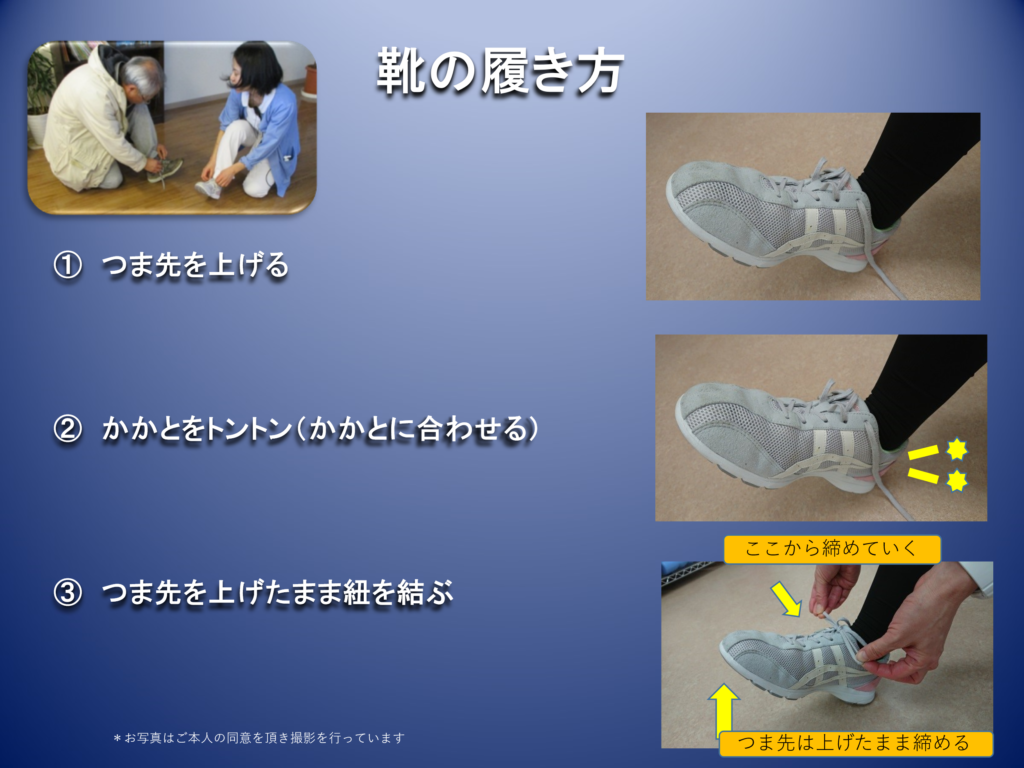
• Initial Visit: Medical examination and foot care guidance. The causes of swelling are investigated, and instructions are given on foot care (stretching, muscle training, proper shoe wear, walking techniques). Follow the pamphlet instructions carefully, as each step is important. Timing and frequency are also crucial.
• One Month Later: Outpatient examination. Symptoms such as pain are expected to reduce by about 20%. Continue at this pace. Confirm whether foot care and walking habits have been established, and provide additional guidance if necessary.
• Four Months Later: Evaluate symptoms and the effects on edema through symptoms and tests. If patients are able to incorporate foot care and walking into their routines, the program is concluded. If insufficient, regular outpatient examinations and guidance continue.
By training and enhancing the flexibility of the intrinsic muscles of the feet and extrinsic muscles from the knee to the foot, we aim to improve the flexibility and strength of the lower leg. Our goal is to achieve the natural shape of the foot, addressing issues such as flat feet and bunions.
Starting with walking for over 30 minutes at least three times a week, ideally daily, is essential.
Fix the heel to the back of the shoe and secure the ankle with laces. This creates space at the toe area, allowing free movement of the toes. Many people leave their laces loose, causing constant pressure on the toes, leading to stiffness. Properly wearing shoes can eliminate toe numbness.
For Patients and Clinic Doctors: Please print and use:
• Foot Care
• Proper Shoe Wear
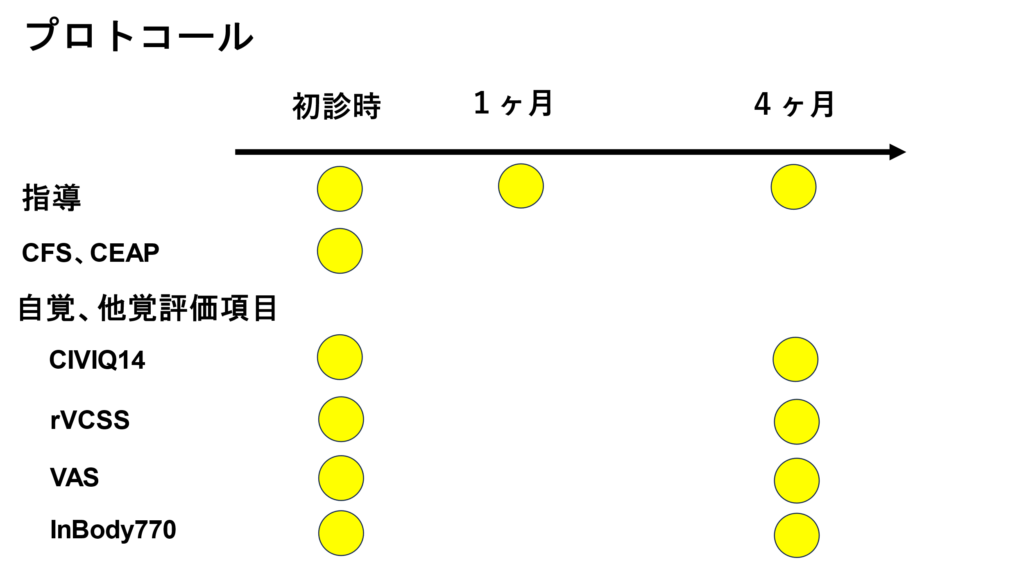
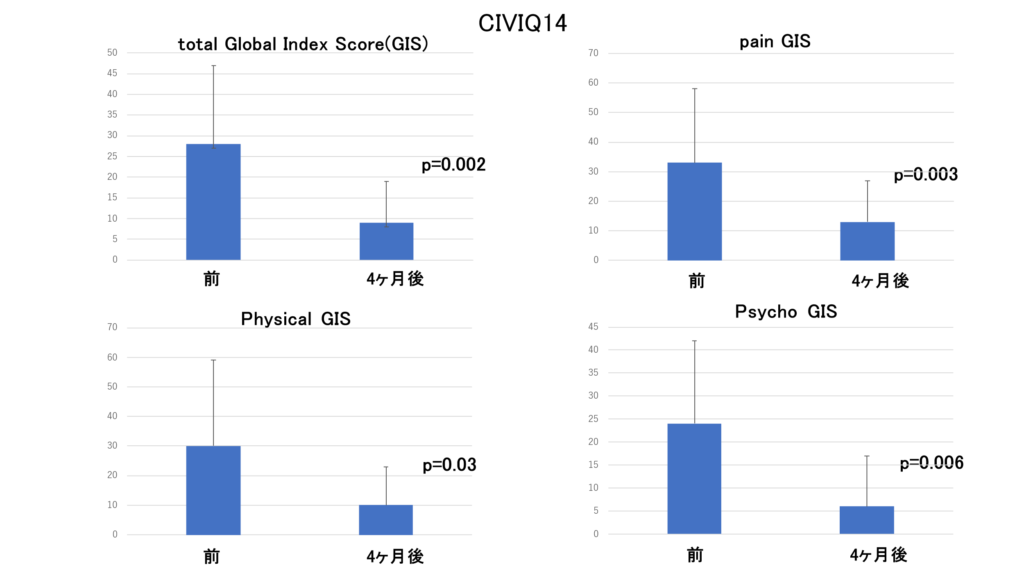
Functional Venous Insufficiency: In 25 cases, the CIVIQ14 (quality of life indicator) showed improvement in pain, physical, and psychological aspects after four months (IRB2023030).
Postoperative Lower Limb Venous Surgery

Postoperative Lower Limb Venous Surgery: Even if venous reflux is stopped through surgery, the lifestyle habits that caused the varicose veins (long hours of standing, lack of exercise) are often still present. This can cause symptoms to persist or reappear a few months after surgery. Improving foot flexibility through stretching and using the muscles by walking are key to achieving truly healthy feet. Starting daily foot care and walking for over 30 minutes at least three times a week, ideally daily, is essential.
Six Months Post-Surgery: Outpatient examination. If symptoms persist and exercise habits are not established, further reinforcement of foot care is conducted.
FAQ
A) Since your current lifestyle has led to your current foot condition, you need to consider additional activities. Please incorporate specific walking for your feet. If you cannot find the time, wear sneakers with properly tied laces even at work. Correctly tying laces can reduce toe strain, even in safety shoes. Farm boots do not facilitate proper foot movement, leading to ineffective muscle pump action and potential toe curling inside the boots.
Q) I don’t know how to walk properly even if I am told to walk.
A) Walking at a pace that feels comfortable or slightly challenging is good for your heart and lungs. Establishing the habit is essential. If your goal is weight loss, start by walking for 10 minutes to warm up, then alternate between 5 minutes of brisk walking and 10 minutes of slow walking. Aim for a total of 60 minutes of brisk walking per week for efficient fat burning.
Q) My knees hurt, and I am seeing an orthopedic doctor. How should I walk?
A) If you have orthopedic issues like osteoarthritis or spinal stenosis, consult your orthopedic doctor on how much walking is appropriate. Also, avoid unstable footwear, as it can lead to further misalignment in your feet, knees, and pelvis. Proper footwear is crucial.
Q) I had surgery and no longer have symptoms. Do I still need to do foot care?
A) Even if venous reflux is stopped through surgery, the lifestyle habits that caused the varicose veins (long hours of standing, lack of exercise) are often still present. This can cause symptoms to persist or reappear a few months after surgery. Foot care and walking are effective for functional venous insufficiency.
Q) I came to the hospital expecting to be cured with medication, but I am only told to do rehab on my own. Will it really help?
A) Clinical research has shown that patients with functional venous insufficiency experienced reduced swelling and symptoms after four months of the foot care program (Gifu Heart Center IRB 2023030). This condition cannot be cured with medication or injections. Improving your daily lifestyle is essential. Take the first step and imagine yourself feeling better in four months. The effort you put in will pay off, and we will support you along the way.
Q) I have already been doing various stretches at the gym. Why do I need this foot care program?
A) Each action, frequency, and duration in this program is meaningful. The stretches and training for your core are different from those for your feet. Let’s work together on foot-specific care.
Q) Can cycling at home replace this program?
A) While cycling provides an exercise load, the action of firmly grounding your feet and supporting your body weight is crucial for foot health. Cycling does not substitute the benefits of walking for foot health.