Peripheral Artery Disease and Venous Disease
Blood vessels are comprised of arteries and veins. In our peripheral vascular clinic, we mainly handle peripheral artery disease (PAD), while venous diseases (such as chronic venous insufficiency, deep vein thrombosis, and varicose veins) are diagnosed and treated in our leg clinic.
Regarding arterial diseases, we primarily address lower extremity artery disease (LEAD) through comprehensive treatment involving catheter interventions favored by internists and bypass or thrombendarterectomy surgeries favored by vascular surgeons.
For venous diseases, varicose veins are treated in our varicose vein clinic, while lymphedema and venous insufficiency are managed in our leg clinic.
We are also equipped to promptly perform balloon angioplasty and thrombectomy for dialysis patients with shunt stenosis or occlusion in collaboration with cardiologists and vascular surgeons.
Chronic limb-threatening ischemia (CLTI), often seen in dialysis patients, requires a multidisciplinary approach. Our Heart Center Group collectively manages these cases, working closely with plastic surgeons to offer the best treatment options for patients.
Peripheral Artery Disease (PAD)
The saying “A man is as old as his arteries” was coined by the 19th-century internist William Osler. This idea, highlighting the progression of arteriosclerosis throughout the body with age, has proven to be accurate. When blood flow is impaired, various symptoms appear in different areas. Peripheral arteries primarily refer to the arteries in the limbs, abdomen, and neck. Diseases caused by occlusion or stenosis of these arteries are collectively referred to as peripheral artery disease (PAD). Particularly, occlusion or stenosis in the leg arteries often presents noticeable symptoms, leading PAD and LEAD to be used interchangeably.
Symptoms of Peripheral Artery Disease (PAD)
intermittent claudication
Intermittent claudication is characterized by fatigue, pain, or numbness in the legs during walking, which prevents continued walking. As leg muscles require more blood flow (oxygen) during walking, symptoms of blood flow insufficiency, such as pain, manifest. These symptoms improve after resting for a while, allowing the resumption of walking.
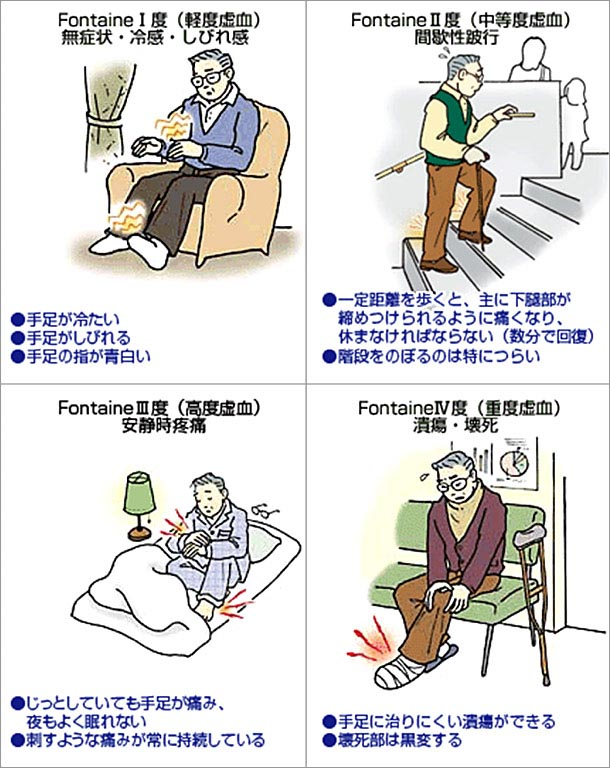
Rest Pain
In more severe cases, pain and numbness can be felt even at rest.
Non-Healing Wounds and Gangrene
In the most severe cases, small wounds that would typically heal in a few days do not heal for weeks (non-healing wounds), and tissues such as skin and muscles die (gangrene). In such conditions, bacterial infection of the wound is common, and limb amputation may become necessary to save the patient’s life. Rest pain, non-healing wounds, and gangrene are collectively referred to as critical limb ischemia.

Treatment of Peripheral Artery Disease (PAD)
Exercise Therapy and Medication
In mild cases of intermittent claudication, symptoms can be improved through exercise therapy (claudication training) and medication, even if arterial stenosis or occlusion remains. Research has shown that supervised exercise therapy is more effective than independent exercise by the patient. Our hospital actively promotes supervised exercise therapy through outpatient visits or short-term hospitalizations. Patients diagnosed with PAD at other hospitals are also welcome to consult us for exercise therapy.

Revascularization (Endovascular Treatment and Surgery)
To improve symptoms of severe intermittent claudication and critical limb ischemia, it is necessary to physically increase blood flow. Endovascular treatment (EVT), also known as catheter treatment, involves expanding the arterial occlusion or stenosis from within the vessel using balloons or stents to repair the artery. The major advantage of EVT is that it can be performed under local anesthesia without the need for skin incisions or sutures, minimizing the body’s trauma.
Surgical treatments for leg arteries include bypass surgery and thrombendarterectomy.

EVT is selected for cases where reocclusion is likely, or greater blood flow improvement is desired. Recent advances in EVT techniques, the development of balloons and stents with lower recurrence rates, and the increasing number of elderly patients have led to a preference for the less invasive EVT. Our hospital offers both EVT and surgical options, allowing us to propose the most appropriate treatment plan based on the patient’s condition. Additionally, with the cooperation of plastic surgeons, we are enhancing our management of patients requiring limb amputation and wound care for non-revascularizable cases.
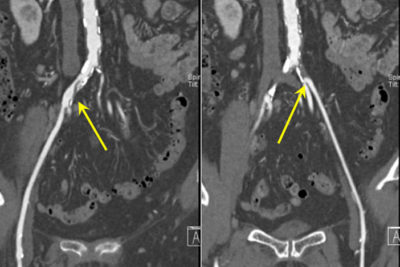
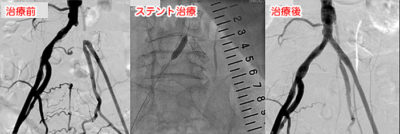
Endovascular Treatment (EVT): Successful revascularization using balloon and stent treatments for the occlusion stenosis indicated by the arrows
Leg Bypass Treatment
Stent graft for superficial femoral artery
Treatment for Venous Disease
For the treatment of varicose veins
please refer to the varicose vein clinic page.
Catheter Treatment for Vascular Access for Hemodialysis (VAIVT: Vascular Access Intervention Therapy)
Vascular access (VA) for hemodialysis, previously known as a dialysis shunt, has become recognized as an access for hemodialysis with the spread of VAIVT (vascular access intervention therapy).

Excerpt from the Basic Techniques Guidelines for Vascular Access Intervention Therapy (VAIVT) for Hemodialysis Vascular Access, revised in May 2020
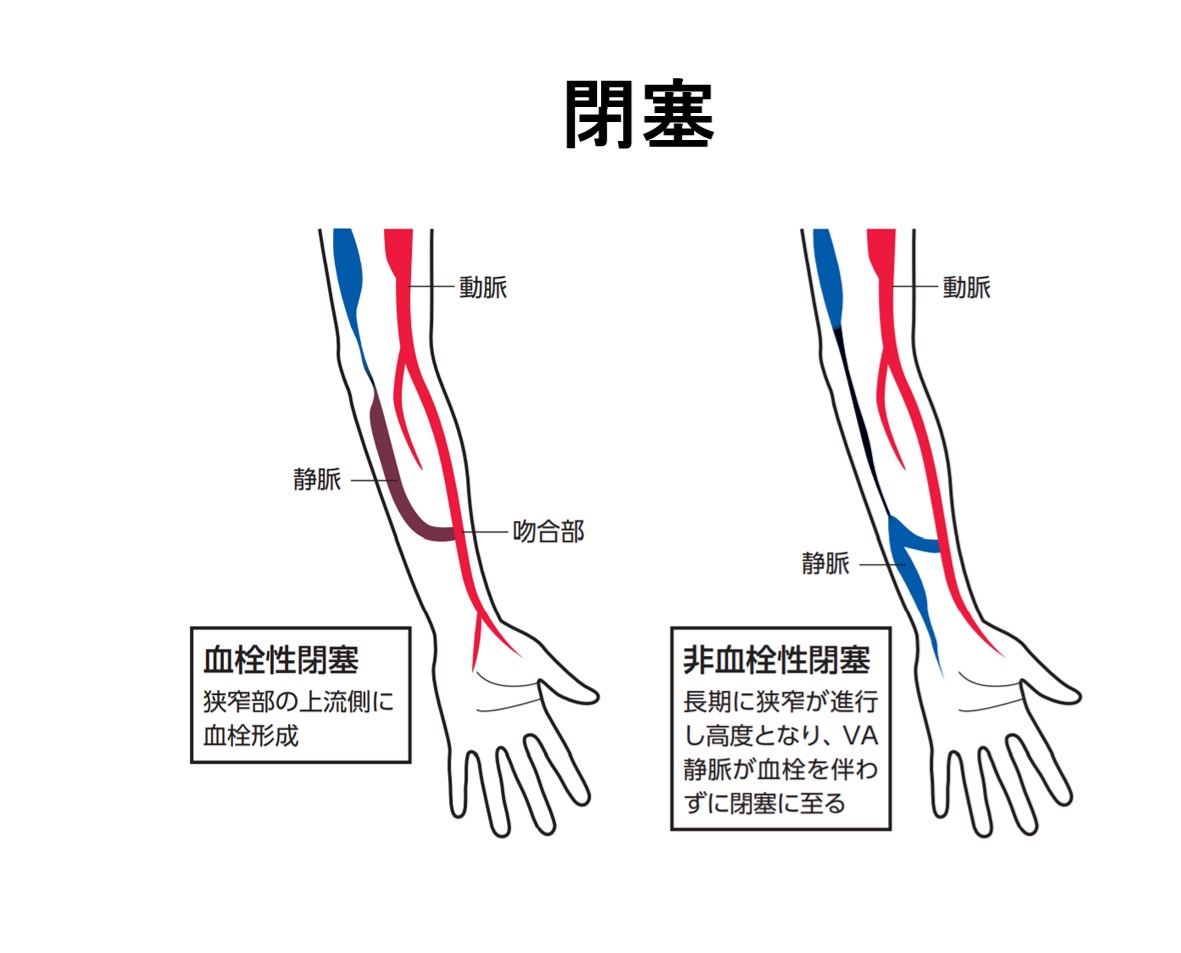
As of the end of 2019, there were over 344,640 maintenance hemodialysis patients in Japan.Diabetic nephropathy is the leading cause of their underlying diseases, accounting for 39.1%, with the average age of patients being 69.1 years, reflecting an aging population. About 90% of vascular access used in Japan are autologous arteriovenous fistulas (commonly called “shunts”), with the remaining 10% being graft fistulas using artificial vessels, arterialization, or long-term indwelling catheters. Autologous arteriovenous fistulas involve connecting an artery to a vein to allow arterial blood to flow into the superficial vein, leading to venous arterialization and repeated needle punctures for hemodialysis three times a week. This process often causes problems due to intimal hyperplasia and stenosis caused by scarring. VAIVT is the primary choice of treatment for maintaining VA function over the long term, depending on the location of stenosis or occlusion.
For venous diseases, we offer a comprehensive range of treatment options, including balloon angioplasty, stent placement, and radiofrequency ablation for varicose veins, to provide the best treatment based on each patient’s condition.

