At our hospital, we treat varicose veins of the lower limbs with various methods including endovenous embolization (Venaseal), endovenous ablation, sclerotherapy, high ligation, and vein stripping. We primarily perform these treatments as outpatient procedures, making it convenient for those with busy work schedules or child care responsibilities who cannot stay overnight. While we require patients to take the day of surgery off from work, our goal is to have them return to work the following day. We conduct a follow-up visit approximately one week after surgery to check the surgical site. Varicose veins can develop due to lifestyle factors such as prolonged standing, sedentary work, and the use of safety boots or rubber boots. To address these factors, we provide guidance on our Gifu Heart Center-developed foot care program. Continuation of this program can help minimize residual symptoms. We also conduct a follow-up visit six months post-surgery to ensure there are no remaining symptoms or varicose veins.
We offer guidance on proper shoe selection, fitting, and walking techniques, which are not typically taught in schools or hospitals. We also provide instructions on the use of compression stockings, elastic bandages, and drainage to help reduce swelling and improve or maintain walking function. Our outpatient foot care team, including certified foot care specialists, compression stocking conductors, and outpatient nurses, work closely with our physicians to support our patients.
Treatment for Varicose Veins according to your medical condition
Understanding Varicose Veins of the Lower Limbs
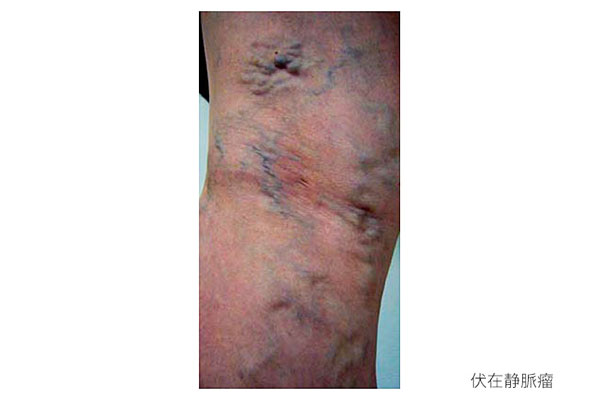
Varicose veins are a condition where the veins near the surface of the legs become enlarged and bulging. They usually appear as soft, blue-purple lumps resembling worms on the lower legs. In some cases, symptoms such as leg numbness may indicate concurrent orthopedic issues like lumbar spondylosis or osteoarthritis of the knee.
About Varicose Veins
Endovenous Radiofrequency Ablation
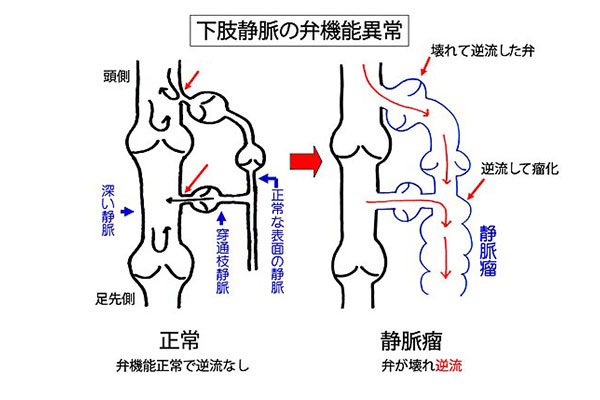
Mechanism of Varicose Vein Formation
Normally, blood circulates from the heart through the arteries to the feet and returns to the heart through the veins. Veins do not have a pump like the heart, so they rely on one-way valves inside them and the contraction of surrounding muscles to push blood back to the heart. These valves prevent backflow, thereby preventing varicose veins. However, if the valves are subjected to pressure and become damaged, backflow can occur in the surface veins, causing them to bulge. Factors such as prolonged standing, genetics, aging, pregnancy, and obesity can contribute to this condition.
Symptoms of Varicose Veins
Symptoms include visible, unsightly veins, leg swelling, fatigue, cramps (charley horses), pain, and itching. Patients often ask what happens if varicose veins are left untreated. We inform them that the condition will not improve on its own and will worsen over the years, potentially leading to complications like thrombophlebitis, which can cause sudden leg swelling. Although it is rare to reach a point of no return, if thrombosis occurs, it can result in redness and swelling (thrombophlebitis) or severe skin discoloration and ulcers that can lead to bleeding and infection. Early surgery is recommended in such cases.
Reasons for Delaying Treatment
Patients often delay treatment because they do not recognize the symptoms as originating from varicose veins due to the chronic nature of the condition, or they are fearful of the word “surgery.” Understanding the treatment process can help alleviate these fears and encourage a more positive attitude towards receiving treatment. Please refer to the following descriptions of various treatment methods.
Types and Treatment of Varicose Veins
- Spider and Thread Veins
ypically treated with conservative methods like compression stockings. However, medical-grade stockings can sometimes be too tight, causing irritation in summer. Therefore, we recommend running tights from sports shops for those who stand for long periods. We also encourage movements that engage the calf muscles, such as tiptoeing and fidgeting. While these measures can be used by those hesitant about surgery, they only prevent worsening and do not cure the condition.

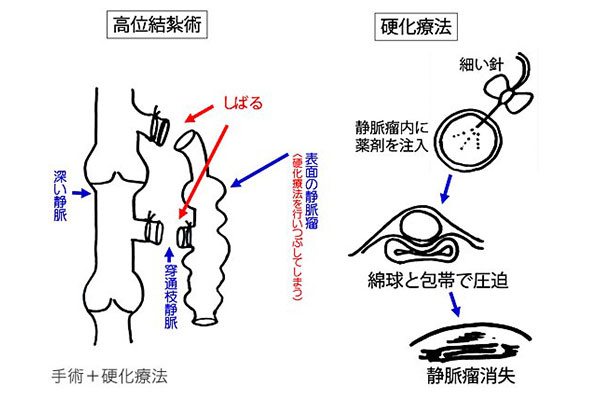
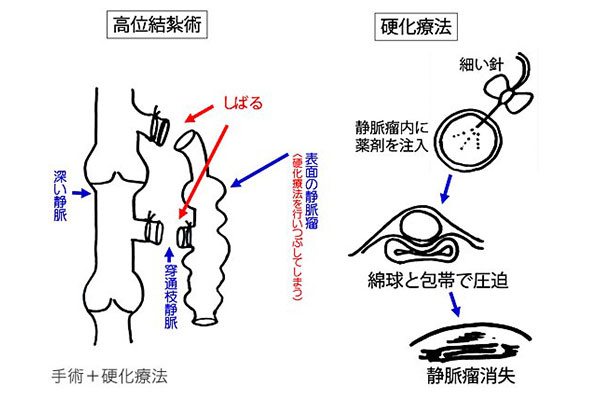
- Sclerotherapy
Developed using various sclerosing agents, sclerotherapy was once less favored due to high recurrence rates. However, in 2000, Tessari developed a simple method of creating foam by mixing polidocanol with air (carbon dioxide and oxygen), which increased the clinical efficacy and led to its widespread use. Suitable for:
1. Thin veins like spider and thread veins
2. Post-surgery recurrences
3. Atypical varicose veins (e.g., varicose veins of pelvic origin)
4. Coronary vein dilations (small varicose veins around the ankles)
Method: A mixture of polidocanol and air is injected as foam into multiple sites using a winged needle. Patients wear compression stockings post-procedure. Additional treatment may be considered if varicose veins persist after 3-6 months.
Side Effects: Pigmentation, pain, and swelling
- Veins Larger than 3mm
Varicose veins due to valve insufficiency in the great saphenous vein (from the groin) or small saphenous vein (from the back of the knee) are treated as follows:
1. Great Saphenous Vein
o Endovenous Embolization (Venaseal)
o Endovenous Ablation
o High Ligation
o Vein Stripping
2. Small Saphenous Vein
o Endovenous Embolization (Venaseal)
o High Ligation
Endovenous Embolization (Venaseal)
pproved in Japan in December 2019 and covered by insurance, this new treatment method was first introduced in Gifu Prefecture by Gifu Heart Center, achieving 500 cases by 2023. Since its introduction in 2020, no severe complications (deep vein thrombosis, pulmonary embolism, stroke, anaphylactic shock, sepsis, granulomatous lesions) have occurred (as of February 2024).

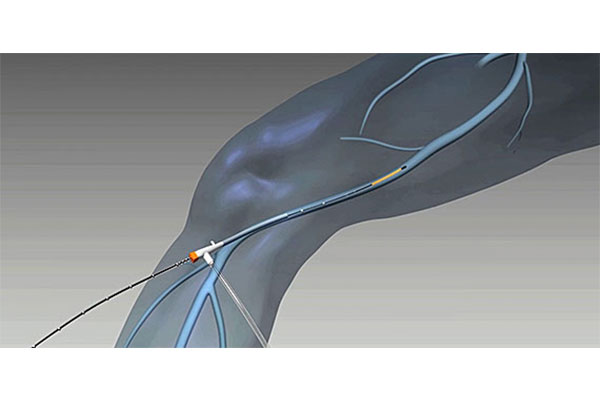
Procedure: After local anesthesia at the insertion site on the inner knee, a thin catheter is inserted into the vein and adhesive is injected to close the vein. Compared to traditional endovenous ablation (laser treatment, radiofrequency treatment), this method has several advantages:
- 1. No heat, reducing the risk of pain and burns2. No need for extensive local anesthesia around the vein
3. No need for post-operative compression stockings
4. No medication restrictions
Note: This method may not be suitable for certain vein locations or shapes, and it is not recommended for patients with a history of deep vein thrombosis, allergies to cyanoacrylate, multiple allergies, allergy medication use, collagen diseases, or granulomas. Although concerns were initially raised about leaving foreign material in the body, recent findings show it decomposes over time
- 1. Insert a catheter into the vein.2. Guide the catheter under ultrasound.
3. Inject adhesive from the catheter.
4. The adhesive solidifies with the blood in the vein.
5. Apply a bandage to the insertion site and finish.
Procedure Steps:
1. Insert a catheter into the vein.

2. Guide the catheter under ultrasound.

3. Inject adhesive from the catheter.
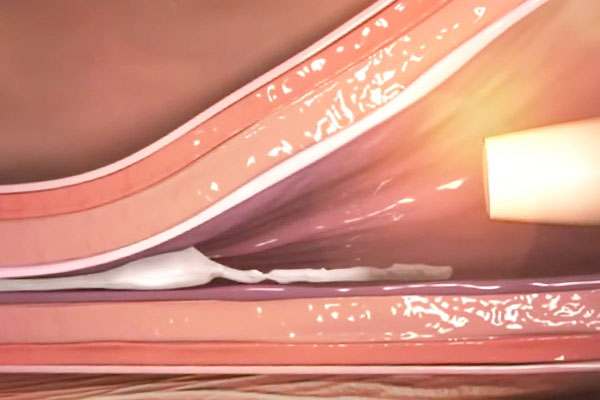
4. The adhesive solidifies with the blood in the vein.

5. Apply a bandage to the insertion site and finish.
資料提供:コビディエンジャパン株式会社
Surgery Schedule
- Pre-operative evaluation in the outpatient clinic to assess varicose veins and overall health, determine the necessity of surgery, and schedule the operation.
- Same-day surgery as an outpatient procedure. Patients are admitted an hour before the scheduled surgery. Local anesthesia is used, and most patients experience only minor pain from the anesthesia injection (similar to a blood draw). We play requested music to help patients relax during the procedure, which typically takes 30 minutes to an hour for one leg.
- After 15 minutes of rest, patients walk to ensure there are no issues and then go home. Normal activities can resume immediately. Extended rest can increase the risk of deep vein thrombosis. We recommend observing the surgical site at home the following day. For those uncomfortable with self-checks, we offer an overnight stay with staff assistance the next morning. Showers are permitted starting the night of the second day post-surgery.
- Follow-up visit one week later to confirm no issues via ultrasound. Bathing is allowed after this visit.
- Lifestyle factors like prolonged standing, sedentary work, and wearing safety or rubber boots are common causes of varicose veins. We provide guidance on a foot care program developed by Gifu Heart Center to help mitigate symptoms.
- Follow-up visit six months post-surgery to ensure no remaining symptoms or varicose veins.
- Treated veins generally close off and disappear over six months to a year. Some tightness and discomfort may persist during this time.
Post-Surgery Restrictions
- Light exercise and work can resume the next day.
- Avoid strenuous activities (marathons, mountain climbing, weight training) for seven days.
- Showers are allowed starting the night of the second day post-surgery, and baths are permitted after the next follow-up visit.
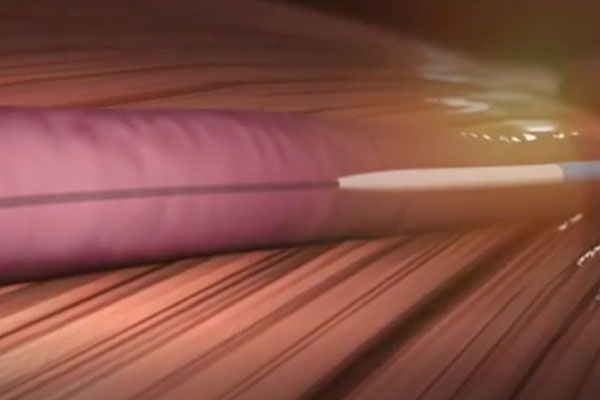
Endovenous Radiofrequency Ablation
ince 2011, endovenous laser treatment for varicose veins has been covered by insurance. We use a high-frequency catheter (ClosureFast™) for endovenous ablation. This method coagulates and closes varicose veins at a lower catheter temperature (up to 120°C), making it a less invasive and safer treatment option compared to endovenous embolization.
資料提供:コビディエンジャパン株式会社
Procedure Steps
- Pre-operative evaluation to assess varicose veins and overall health, determine the necessity of surgery, and schedule theoperation.
- Same-day surgery as an outpatient procedure. Local anesthesia is used, and patients experience minimal pain after the initial anesthesia injections. We play requested music to help patients relax during the procedure, which typically takes 30 minutes to an hour for one leg. Patients return to their room with bandages after the procedure.
- After 15 minutes of rest, you will walk to confirm there are no issues, and then you can go home. There is no need to rest after returning home; you can live as usual. Resting excessively could lead to the formation of deep vein thrombosis or other complications. (This is typically a same-day procedure.) The next day, you will observe the surgical site at home, remove the bandages, and wear compression stockings. If you feel uneasy about putting on the stockings by yourself, you may opt for a one-night stay. In that case, the staff will assist you the morning after the surgery. You can take a shower starting the night two days after the surgery. You will need to wear the compression stockings for about two weeks post-surgery.
- About one week later, you will visit the outpatient clinic for an ultrasound examination to ensure there are no problems. You will be allowed to take a bath (soak in the tub).
- Common causes of varicose veins include lifestyle factors such as standing or sitting for long periods, wearing safety shoes, and boots. To address these, we provide foot care program guidance developed by the Gifu Heart Center. Continuation of this program tends to reduce the remaining symptoms.
- After six months, you will visit the outpatient clinic to check for any remaining symptoms or varicose veins.
- Generally, the treated veins will be closed and disappear over six months to a year. During this period, you may still experience a feeling of tightness or lumpiness.
High Ligation Surgery
This involves making several 1-2 cm skin incisions under local anesthesia (the number and location vary depending on the condition). By tying off the root of the vein with damaged valves, we stop the blood from flowing backward. If necessary, we inject a sclerosing agent into the remaining varicose veins. At our hospital, we perform an ultrasound examination of the superficial veins just before the surgery to accurately identify and ligate the veins with reflux (including not only the root but also the perforator veins). This method is especially effective when the varicose veins are large, and other treatments (such as endovenous laser ablation or embolization) are unsuitable. We choose high ligation surgery as the first option for the small saphenous vein, where there is a risk of nerve damage due to the close proximity of nerves. The back of the knee is an area that bends with the joint, so there is a risk of recurrence if you habitually sit on your knees.
High Ligation Surgery
This procedure is performed when the vein is large and accompanied by thrombosis. In the past, spinal anesthesia was required, and a few days of hospitalization were necessary. Nowadays, the procedure can be done as day surgery using TLA anesthesia.

